Abstract
BACKGROUND: Secondary acute myeloid leukemia (AML) is defined as AML that develops from a prior myelodysplastic or myeloproliferative disorder, or from exposure to chemotherapy, radiation, or environmental toxins. Patients with secondary AML have inferior prognosis compared to those with de novo AML,1 and are more likely to be elderly with increased comorbidities and worse performance status.2 The detection of minimal residual disease (MRD) also has independent prognostic value in patients with AML.3-6 In elderly AML patients, MRD predicts worse outcomes independent of the poor treatment risk factors associated with increased age.7Due to the similar disease pathogenesis between elderly AML and secondary AML patients, it is likely that MRD testing will have similar implications. However, there is limited data on the prognostic role of MRD testing in secondary AML.
METHODS: We retrospectively analyzed de novo and secondary AML patients at Washington University Medical Center who received post-induction, post-consolidation, pre-transplant, or post-transplant MRD testing during their treatment. MRD testing was performed with multiparameter flow cytometry testing using the "different from normal" method at one reference laboratory,8,9 with positive MRD defined as detection of an abnormal myeloblast population above 0.1%. A total of 180 patients were included. Any patient with at least one positive MRD was considered "MRD positive." Baseline pretreatment characteristics were compared between groups with Mann-Whitney, Chi-square, or Fisher's exact test, when appropriate. We evaluated overall survival (OS) and relapse rates in de novo and secondary AML patients stratified by MRD status using Kaplan-Meier curves and the log rank test, or cumulative incidence function, as appropriate. Multivariate Cox proportional hazards model was also fitted to determine if MRD testing has similar prognostic value across de novo and secondary AML patients.
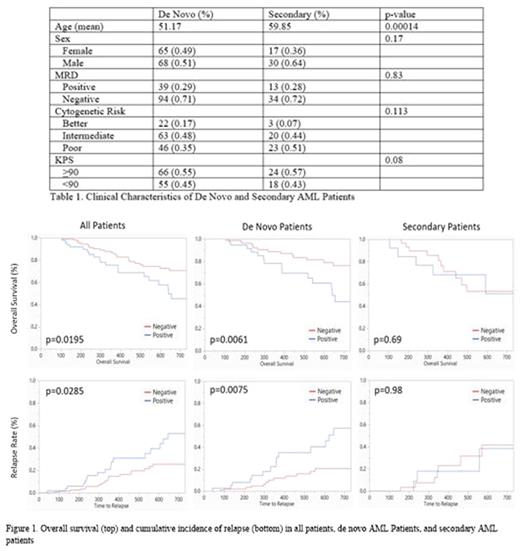
RESULTS: Our analysis included 133 patients with de novo and 47 patients with secondary AML. Secondary AML patients were significantly older at age of diagnosis (mean age 59.85 versus 51.17, p<0.001), however had similar rates of MRD positivity (28% versus 29%, p=0.830). There was a trend toward poorer cytogenetic risk profiles and worse Karnofsky Performance Status in secondary AML (Table 1). In all patients, we confirmed that MRD positivity confers significantly worse OS (45.5% versus 70.8%, p=0.020) and relapse rates at 2 years (53% versus 25.5%, p=0.029) (Figure 1). In de novo AML patients, MRD positivity continued to demonstrate significantly worse 2-year OS (44.1% versus 76.3%, p=0.006) and relapse rates (57.6% versus 20.7%, p=0.008). However, in secondary AML patients, there were no differences in OS (p=0.69) or relapse rates (p=0.98) between MRD positive and negative patients. Multivariate analysis demonstrated significant interaction (p=0.042) between MRD status and AML subtypes. MRD positivity emerged as an independent prognostic indicator of worse OS in de novo patients (HR 2.8, 95% CI 1.524-5.405) but not in secondary patients (HR 1.5, 95% CI 0.188-2.336).
DISCUSSION: We confirm that MRD status is a poor prognostic indicator in all AML patients, and this also holds true in patients with de novo AML. However, we found that MRD status has less prognostic value in secondary AML patients. This may be due to the overall poor prognosis seen in secondary AML patients, suggesting that MRD monitoring in this group of patients may be less useful for risk stratification. However, our study is limited by the small sample size, particularly in the number of secondary AML patients who displayed MRD positivity (N=13). In addition, we defined MRD positivity across all time points of testing, which may decrease patient homogeneity. A larger study with increased follow-up is necessary to confirm our findings, as these results have important implications in risk-stratification and treatment of patients with secondary AML.
DiPersio: BMS, Asterias, Amphivena, Bluebird: Other: Travel, Accomodations, Expenses; Hemedicus, DAVA Oncology: Speakers Bureau; Celgene, Bioline, Vasculox, Cellworks, Rivervest: Consultancy; Magenta Therapeutics: Equity Ownership.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal